India’s historical lockdown is now in its sixth week. It all started with an appeal from the Prime Minister, Narendra Modi to observe 14-hours voluntary Janta curfew on 22nd March 2020. Further, on 24 March 2020, the Prime Minister ordered the nationwide lockdown for 21 days, affecting 1.3 billion people of India. As India was settling down under the ongoing strain of lockdown, on 14 April, the Prime Minister again appeared on television. This time in a white kurta, covering his mouth with Assamese gamcha (a cloth used by Indian rural men) With his usual flourish and exceptional rhetoric, he announced lockdown to be extended till 3rd May. India’s fragile healthcare infrastructure and catastrophic threats of COVID-19 left very little choices to exercise.
The world is grappling with a pandemic that is unprecedented in its scale and intensity. The Worldometer reported around 3.8 million cases and 0.26 million deaths around the globe. Whereas the number in India is concerned, until today, there are more than 52,000 cases and more than 1,700 deaths. Cases are getting doubled in 10.2 days. In some parts, the number is increasing at a much quicker pace. Though the impact of the pandemic reached a little late in India, Intensity is not at all less severe.
Health Care Infrastructure
Every failure or unexpected moment in life offers an opportunity to introspect our own behavior and so the ongoing COVID-19 pandemic is the perfect time to introspect on the healthcare system in India. Though there are numerous parameters that could be attributed to healthcare infrastructure, this article intends to cover the number of doctors, availability of hospital beds, acute care beds per 1,000 population.
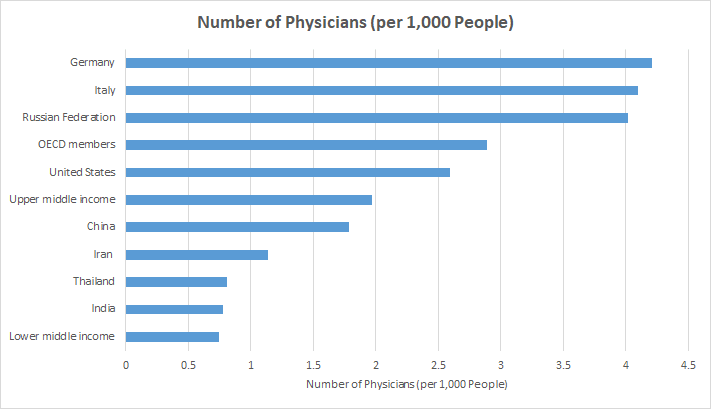
Doctors, nurses, and other healthcare staffs are the backbone of health care infrastructure. The quality care and promptness of its services primarily depend on the number of healthcare professionals in any country. Considering the number of physicians (per 1,000 people), as per the report, India reported 0.78 physicians in 2017 based on its population in that year. The number is lower than the World Health Organization’s (WHO) desirable doctor–population ratio as 1:1,000. Though the number is in par with other lower-middle-income economies (GNI per capita between $1,026 and $3,995); however, it is significantly lower than that of upper-middle-income (1.971) and high-Income economies (3.004).
The number of available hospital beds in another important indicator to understand the healthcare infrastructure. In association with the National Health Profile-2019, The Brookings Institution estimates 7,13,986 total government hospital beds available in India. It translates to 0.55 beds per 1,000 population. The report says there are many states that lie below the national level figure (0.55 beds per 1,000 population). These include Bihar, Jharkhand, Gujarat, Uttar Pradesh, Andhra Pradesh, Chhattisgarh, Madhya Pradesh, Haryana, Maharashtra, Odisha, Assam and Manipur. Bihar has an acute shortage of government hospital beds with just 0.11 beds available per 1,000 population. West Bengal, Sikkim, Delhi, Kerala, Tamil Nadu are equipped well in terms of hospital beds and number is proportionately higher than the national average.
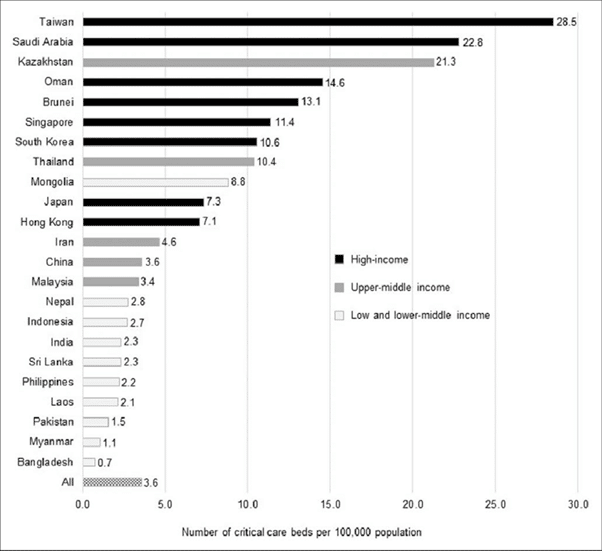
The number of government hospital beds is low, and the current situation of the ongoing COVID-19 pandemic is likely to have a detrimental effect on patients requiring critical care. Let’s have look at the availability of critical care beds. As per the report, around 6.1% of COVID-19 patients are critical with respiratory failure. Such patients require intensive care unit. As the greater number of COVID-19 patients emerges, the number of required critical beds would rise proportionately. A recent study on critical care bed capacity in Asian countries estimate that there are merely 2.7 beds per 100,000 people in India which is considerably lower than South Korea (10.6), Thailand (10.7), Mongolia (8.8), Japan (7.3), Iran (4.6), and the comparison does not end without comparing with China (3.6).
Healthcare Expenditure
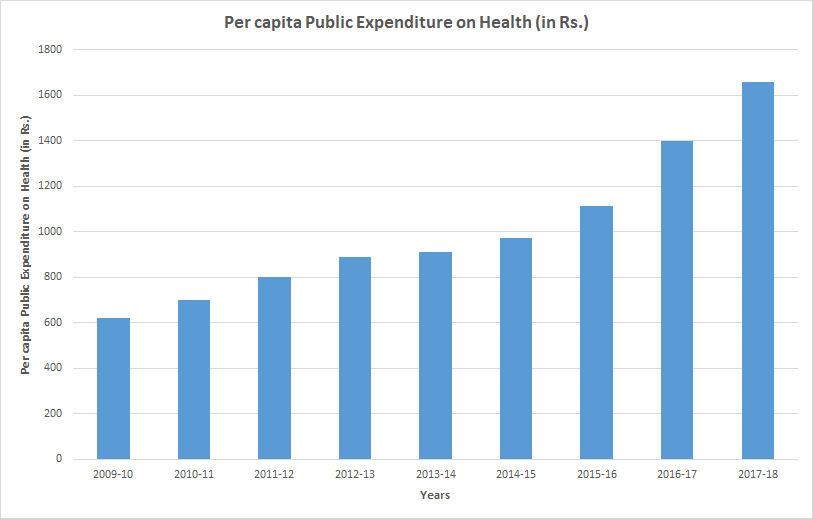
On the earthly planet, resources depend upon how much money is spent. It is important to have a glance at public and out-of-pocket spending in India’s healthcare sector. As per the National Health Profile-19, Government expenditure is 1.28% of its GDP (2017–18 Budget estimates). This expenditure was 1.02% in 2015-16 and there was almost no change in number from 2009-10. It is also reported to be among the lowest in the world for low-middle-income countries. The total per capita government spending on healthcare has nearly doubled from ₹1,008 per person in FY15 to ₹1,944 in FY20 but is still low. Another issue: spending is fragmented among union and state levels. The Centre: State share in total public expenditure on health was 37:63 in 2017-18.
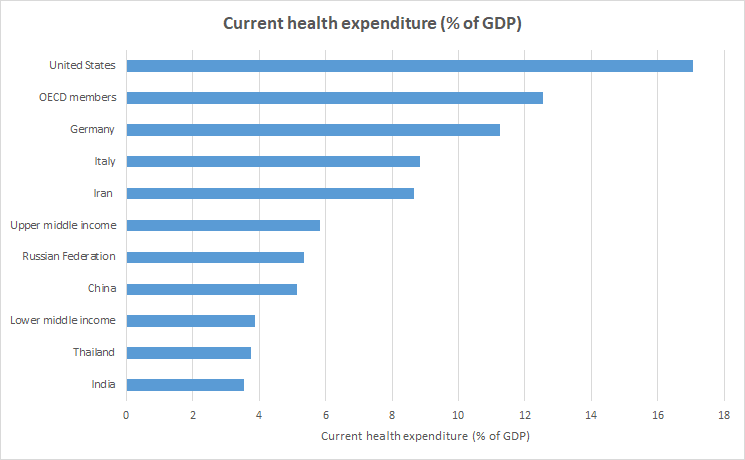
India’s total health care spending taking account of out-of-pocket and public is 3.6% of GDP, as per the World Bank data. The number for the year 2017 is in par with lower middle-income economies; however, significantly lower than that of upper middle-income economies (5.84), OECD countries (12.55).
With the rise in the cost of treatment, as observed by the National Health Profile-2019, it has led to inequity in access to health care services. Moreover, with the constrained public healthcare contribution, out-of-pocket expenditure is high in India. Due to elevated levels of fragmentation in the sources of revenues, the most health expenditure (about 64 %) coming directly from households, out-of-pocket. The out-of-pocket expenditure for china is just 36% of the total healthcare expenditure. The effect of these rippled and push a considerable number of households below the poverty line.
India also experiences fragmented delivery of healthcare services, health financing, and risk pooling. Health care services are completely fragmented. Over 98% of healthcare facilities in India are those which employ ten persons or less. This causes health records of patients to remain buried in manual systems or left unused for cross-sharing for the framing of public policy and research.
How critical health system transformations can help
Based on economic calculations by Ajay Mahal and Cristian Baeza, by introducing critical health system transformations, India can save more than a million additional children’s lives and reduce working-age adult’s death by an additional 16% and that will have a consequential impact on increased real GDP 64% by 2030. At the same time, it will help to reduce out-of-pocket expenses which will save at least 1.5 million additional households from falling into poverty due to illness. Further, such a system will Improve consumer experience and citizen satisfaction. It is also expected to offer a globally competitive healthcare insurance and service provision industry which will have a substantial impact on employment and help India to emerge as a place of medical tourism.