What’s the difference between miscarriage and stillbirth?

What’s the difference? is a new editorial product that explains the similarities and differences between commonly confused health and medical terms, and why they matter.
Former US First Lady Michelle Obama revealed in her memoir she had a miscarriage. UK singer-songwriter and actor Lily Allen has gone on the record about her stillbirth.
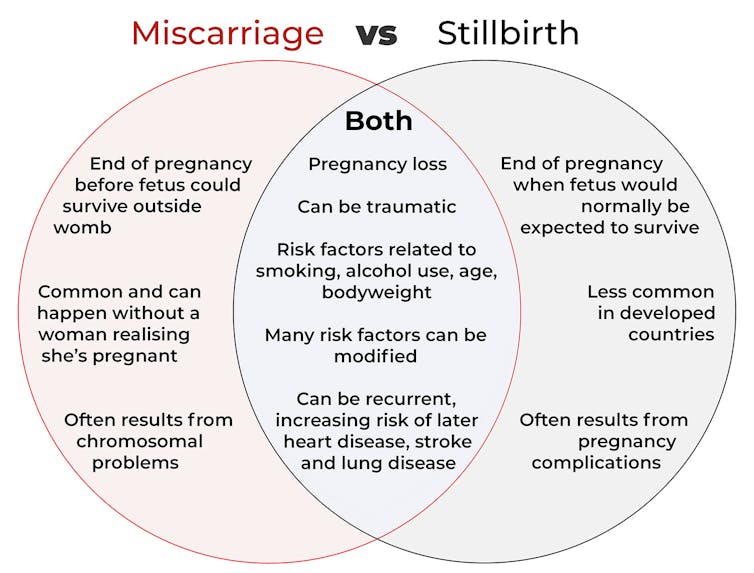
Both miscarriage and stillbirth are sadly familiar terms for pregnancy loss. They can be traumatic life events for the prospective parents and family, and their impacts can be long-lasting. But the terms can be confused.
Here are some similarities and differences between miscarriage and stillbirth, and why they matter.
Let’s start with some definitions
In broad terms, a miscarriage is when a pregnancy ends while the fetus is not yet viable (before it could survive outside the womb).
This is the loss of an “intra-uterine” pregnancy, when an embryo is implanted in the womb to then develop into a fetus. The term miscarriage excludes ectopic pregnancies, where the embryo is implanted outside the womb.
However, stillbirth refers to the end of a pregnancy when the fetus is normally viable. There may have been sufficient time into the pregnancy. Alternatively, the fetus may have grown large enough to be normally expected to survive, but it dies in the womb or during delivery.
The Australian Institute of Health and Welfare defines stillbirth as a fetal death of at least 20 completed weeks of gestation or with a birthweight of at least 400 grams.
Internationally, definitions of stillbirth vary depending on the jurisdiction.
How common are they?
It is difficult to know how common miscarriages are as they can happen when a woman doesn’t know she is pregnant. There may be no obvious symptoms or something that looks like a heavier-than-normal period. So miscarriages are likely to be more common than reported.
Studies from Europe and North America suggest a miscarriage occurs in about one in seven pregnancies (15%). More than one in eight women (13%) will have a miscarriage at some time in her life.
Around 1–2% of women have recurrent miscarriages. In Australia this is when someone has three or more miscarriages with no pregnancy in between.
Australia has one of the lowest rates of stillbirth in the world. The rate has been relatively steady over the past 20 years at 0.7% or around seven per 1,000 pregnancies.
Who’s at risk?
Someone who has already had a miscarriage or stillbirth has an increased risk of that outcome again in a subsequent pregnancy.
Compared with women who have had a live birth, those who have had a stillbirth have double the risk of another. For those who have had recurrent miscarriages, the risk of another miscarriage is four-fold higher.
Some factors have a u-shaped relationship, with the risk of miscarriage and stillbirth lowest in the middle.
For instance, maternal age is a risk factor for both miscarriage and stillbirth, especially if under 20 years old or older than 35. Increasing age of the male is only a risk factor for stillbirth, especially for fathers over 40.

Elizaveta Galitckaia/Shutterstock
Similarly for maternal bodyweight, women with a body mass index or BMI in the normal range have the lowest risk of miscarriage and stillbirth compared with those in the obese or underweight categories.
Lifestyle factors such as smoking and heavy alcohol drinking while pregnant are also risk factors for both miscarriage and stillbirth.
So it’s important to not only avoid smoking and alcohol while pregnant, but before getting pregnant. This is because early in the pregnancy, women may not know they have conceived and could unwittingly expose the developing fetus.
Why do they happen?
Miscarriage often results from chromosomal problems in the developing fetus. However, genetic conditions or birth defects account for only 7-14% of stillbirths.
Instead, stillbirths often relate directly to pregnancy complications, such as a prolonged pregnancy or problems with the umbilical cord.
Maternal health at the time of pregnancy is another contributing factor in the risk of both miscarriage and stillbirths.
Chronic diseases, such as high blood pressure, diabetes, hypothyroidism (underactive thyroid), polycystic ovary syndrome, problems with the immune system (such as an autoimmune disorder), and some bacterial and viral infections are among factors that can increase the risk of miscarriage.
Similarly mothers with diabetes, high blood pressure, and untreated infections, such as malaria or syphilis, face an increased risk of stillbirth.
In many cases, however, the specific cause of pregnancy loss is not known.
How about the long-term health risks?
Miscarriage and stillbirth can be early indicators of health issues later in life.
For instance, women who have had recurrent miscarriages or recurrent stillbirths are at higher risk of cardiovascular disease (such as heart disease or stroke).
Our research has also looked at the increased risk of stroke. Compared with women who had never miscarried, we found women with a history of three or more miscarriages had a 35% higher risk of non-fatal stroke and 82% higher risk of fatal stroke.
Women who had a stillbirth had a 31% higher risk of a non-fatal stroke, and those who had had two or more stillbirths were at a 26% higher risk of a fatal stroke.
We saw similar patterns in chronic obstructive pulmonary disease or COPD, a progressive lung disease with respiratory symptoms such as breathlessness and coughing.
Our data showed women with a history of recurrent miscarriages or stillbirths were at a 36% or 67% higher risk of COPD, respectively, even after accounting for a history of asthma.

PRPicturesProduction/Shutterstock
Why is all this important?
Being well-informed about the similarities and differences between these two traumatic life events may help explain what has happened to you or a loved one.
Where risk factors can be modified, such as smoking and obesity, this information can be empowering for individuals who wish to reduce their risk of miscarriage and stillbirth and make lifestyle changes before they become pregnant.
More information and support about miscarriage and stillbirth is available from SANDS and Pink Elephants.
Gita Mishra, Professor of Life Course Epidemiology, Faculty of Medicine, The University of Queensland; Chen Liang, PhD student, reproductive history and non-communicable diseases in women, The University of Queensland, and Jenny Doust, Clinical Professorial Research Fellow, School of Public Health, The University of Queensland
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Observer Voice is the one stop site for National, International news, Sports, Editor’s Choice, Art/culture contents, Quotes and much more. We also cover historical contents. Historical contents includes World History, Indian History, and what happened today. The website also covers Entertainment across the India and World.